Introduction
Coccidia are single-celled, microscopic parasites that live and reproduce in animal cells. Coccidia of sheep are host specific and almost all lambs will become infected in early life with one or more species.
Most of the different species found in sheep are harmless and may even provide beneficial effects. Only two harmful (or pathogenic) species cause clinical disease (Eimeria ovinoidalis and Eimeria crandallis) when there is either a heavy infestation in lambs or they have lowered immunity. Distinguishing between an infection with coccidia and the disease coccidiosis is very important.
Lambs take in pathogenic coccidia oocysts (eggs) by mouth. Inside the gut, the oocysts hatch, invade the gut cells and multiply dramatically. The coccidia emerge by bursting the cells open - damaging the inside lining of the lamb's gut. A dramatic number of oocysts are shed in faeces and this can be many million times higher than the number that were ingested. It takes two to three weeks from infection via the mouth to passing oocysts from the rectum.
On pasture and in buildings the oocysts are very hardy and can survive for long periods including over winter. They are resistant to drying, freezing, heat and many disinfectants. Ewes also shed low numbers of oocysts which can initiate infection even on clean pasture.
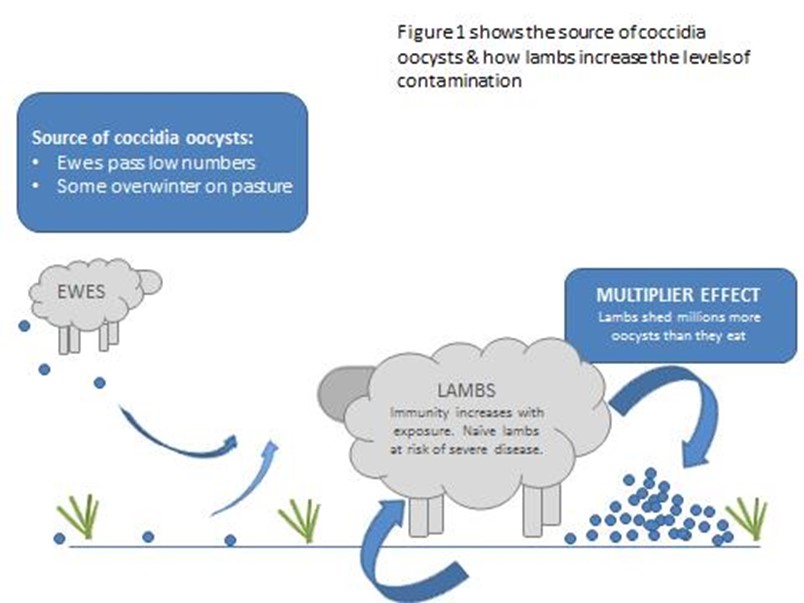
Figure 1. The source of coccidia oocysts.
Clinical Signs
In the UK, clinical coccidiosis is most often seen in lambs aged four to eight weeks old and it is not common in animals over three months old unless they are debilitated. Clinical disease will appear to affect lambs at progressively younger ages as the season progresses on a farm and pasture or building contamination increases.
Significant damage to the cells lining the small intestine, caecum and large intestine results in diarrhoea which may contain mucus or blood. This is often accompanied by straining, pain, weight loss and sometimes death of the lamb. Ongoing poor growth rates may be apparent in older lambs after clinical or subclinical disease as the gut has a reduced ability to absorb nutrients from food.

Figure 2. Common signs of coccidiosis are dullness, rapid weight loss, staining of the back end, straining and diarrhoea containing mucus and blood.

Figure 3. Diarrhoea with mucus from a lamb with coccidiosis.

Figure 4. Diarrhoea and staining with fresh blood is highly suggestive of coccidiosis.

Figure 5. Straining can prolapse the rectum and is often accompanied by painful cries.
Diagnosis
Clinical signs of severe, bloody diarrhoea and straining can be highly suggestive of coccidiosis but the disease should be confirmed. Faecal samples can be taken to identify a significant oocyst count of pathogenic species of coccidia. Samples with a high faecal coccidia count alone may not be significant and they should be speciated to confirm the oocysts are the harmful type at an accredited laboratory. Many lambs have a very high count of harmless oocysts.
In some cases of severe disease or death, oocysts may not be present in the faeces. The diagnosis can be confirmed by post mortem examination findings of severe inflammation of the gut with various coccidia life stages present in gut wall scrapings. Faecal samples taken from a mixture of ten healthy and affected animals in the group can also be used to indicate the presence of high numbers of pathogenic coccidia oocysts.

Figure 6. Diagnosing the causes of diarrhoea using microscopy of faecal samples.
Other causes of diarrhoea and weight loss in older lambs include worms (particularly nematodirosis) and salmonellosis. These diseases can occur concurrently with coccidiosis which is very damaging. Fertilised, lush grass and high protein creep feed can also cause scour. Malnutrition, including vitamin and mineral deficiencies, predisposes lambs to coccidiosis in addition to being a primary cause of poor condition.

Figure 7. Scouring lambs at pasture need a diagnosis to differentiate coccidioisis from other causes - particularly nematodirosis.
Treatment
There are three licensed ingredients available for treating or preventing coccidiosis in sheep - diclazuril (e.g. Vecoxan), toltrazuril (e.g.Baycox, Toltranil and Cavezuril) and decoquinate (e.g. Decoxx).
Decoquinate is an in-feed medication which can only be added to commercial creep feeds by the manufacturer following receipt of an appropriate prescription from the farmers vet. It is incorporated to provide the recommended concentration of 100 mg decoquinate/kg feed (100 ppm) for the duration of the period of risk and fed for a minimum of 28 days.
Each 10kg lamb must ingest 100g of creep a day to maintain adequate decoquinate levels. Sick lambs (e.g. with nematodirosis) with inadequate appetites to eat enough medicated creep are at risk of developing concurrent clinical coccidiosis. Decoquinate is also only active in the small intestine and lambs may still shed oocysts from the large intestine despite eating medicated feed and showing no clinical signs of coccidiosis.
Diclazuril and toltrazuril are oral drenches which can be used for treatment in the face of an outbreak. They should be given to all lambs over three weeks of age in a group where coccidiosis has been diagnosed as the cause of clinical disease. It may be necessary to repeat the diclazuril dose after three weeks.
Lambs with severe diarrhoea and dehydration also require appropriate supportive therapy with oral electrolyte solutions and nursing care. They must be protected from adverse weather and predation, monitored for adequate feeding with supplementation when necessary, and protected from blowfly strike. Any other concurrent disease e.g nematodirosis must be diagnosed and treated.
Prevention and Control
There are two aspects to preventing clinical coccidiosis. The first is eliminating or lowering the numbers of pathogenic oocysts ingested through good biosecurity, hygiene and management. The second is timed and targeted preventative treatment.
There is no cross protection of immunity to different species of coccidia. Maintaining a closed flock or following robust isolation and quarantine procedures can reduce the risk of purchasing animals shedding a novel species.
Prior to lambing and between groups all housing and pen materials should be thoroughly cleaned to remove all organic material and then disinfected with a product effective against coccidia oocysts. Very few disinfectants can kill oocysts so seek advice and check the product claims and concentrations carefully. In housing, the concentration of oocysts contaminating the environment is lowered by reducing stocking density, ensuring adequate ventilation and drainage, and providing regular, plentiful bedding.
At pasture, contamination levels are reduced by regularly moving to clean grazing and avoiding fields that carried young lambs in the previous season when possible. Lambs with ewes at lower stocking densities have a much lower risk of disease. Areas around creep feeders can become heavily contaminated and should be moved onto fresh ground daily.

Figure 8. Poached areas around feed troughs can become heavily contaminated with oocysts in warm, wet weather. Move the hopper to help prevent disease.
Milk feeding equipment, water buckets and feed troughs must be cleaned and disinfected regularly. Water should be from a fresh, clean supply. Elevating buckets and troughs from ground level reduces faecal contamination.

Figure 9. Avoid faecal contamination in and around feed troughs.
Lambs that had adequate colostrum intake have a lower risk of coccidiosis. Twins and triplets have a greater risk. Lambs receiving lower milk volumes graze more at a younger age and ingest a higher level of oocysts earlier in life before adequate immunity develops. Malnutrition through a lack of energy or protein intake, or deficiency of vitamins or minerals increases a lambs susceptibility to coccidiosis. Poor, underfed lambs will have more severe clinical disease than well fed animals with the same level of oocyst challenge.
Other stressors for example extreme weather, transportation, mixing, docking and castrating will lower lambs’ resilience to coccidiosis.
Group treatment to prevent clinical disease can be given when history and screening indicate the lambs will face an expected high coccidia challenge. It is important to understand which lambs are at high risk so appropriate treatment is targeted at these. Such high risk situations include:
- Susceptible lambs are moved onto fields or into a contaminated building where older lambs have been.
- Lambs which have been kept housed in well-bedded, clean conditions for an extended period after birth are turned out onto contaminated pasture.
- Lambs which have been fed on medicated creep feed (or had access to their mothers' medicated feed) if that medication is suddenly withdrawn.
Traditionally decoquinate was used in the ewe ration to suppress the number of oocysts shed by the ewes. However, this blanket approach is no longer recommended for a number of reasons. Firstly, the ewes are medicated despite being clinically unaffected by coccidia. Secondly some of the source of coccidia for the lambs comes from overwintered oocysts on the pasture and medicating the ewes does not remove this. Lastly there are benefits of very young lambs having access to low levels of coccidia to build their own immunity.
Diclazuril has no residual activity so the timing of treatment is critical and it is rarely appropriate to be used on the day of turn-out. When susceptible lambs are moved onto contaminated land, the product should be given 10-14 days later and it may be necessary to give a second dose three weeks after the first.
Toltrazuril has a longer duration of action so one dose is all that is necessary. Timing is less critical but the ideal timing of treatment is a week after turn-out onto contaminated land or a week before expected clinical disease.
Various studies have shown that in the face of a coccidia challenge, lambs treated with either diclazuril or toltrazuril shed fewer coccidia oocysts, have less or no diarrhoea and grow faster than untreated lambs. A single dose of toltrazuril has been shown to be more effective at reducing the numbers of oocysts shed than either a single or double dose of diclazuril, resulting in less contamination of the pasture and a lower challenge facing the next batch of lambs.

