Swine Dysentery has long been recognised as a major disease of pigs throughout the world and can be seen in all types of pig keeping operations.
The causative bacterium was identified back in the 1960's now referred to as Brachyspira hyodysenteriae, but previously known as Treponema and Serpulina hyodysenteriae.
Dysentery, as a pathological condition, is typified by bloody diarrhoea and in its original form this is how the disease presented in pigs. However, Brachyspira hyodysenteriae is not the only cause of bloody diarrhoea in the pig, but conversely it is now recognised that not all strains of Brachyspira hyodysenteriae cause classic signs of Swine Dysentery.
Clinical Presentation
The typical pig affected with swine dysentery will appear dull, depressed and inappetant with sunken (or slab) sides to its abdomen.
Dehydration is common. The faeces will range from soft to almost water, containing blood, mucous and in severe cases necrotic gut lining. (Fig 1 & 2). It will give off a distinctive and unpleasant smell. The disease runs over a number of days, with initially raised rectal temperatures up to 41°C (106°F) but this will fall over a few days. Death can result early on or later and may itself be the result of dehydration/salt poisoning.

Fig 1: Typical faeces from a pig with Swine dysentery (SD)

Fig 2: Loss of condition and faeces stained perineum are features of Swine Dysentery
As a group disease, signs will spread steadily within and between pens over a number of days - rather than explosively. Untreated and uncontrolled, the disease will persist within dynamic production systems for prolonged periods of time, if not permanently, whereas in fixed populations survivors that fully recover will throw off infection over time and the disease can eventually burn itself out.
In a naïve population, the disease can occur in all age groups of pigs - as young as 2-3 weeks of age and in adults. However, it is most typically a disease of the growing pig above 12 weeks of age and in chronically infected herds disease is often restricted to this age group.
Diet can have dramatic effects on the severity of the disease and some studies have shown that even in the face of severe challenge, pigs fed on cooked white rice show little sign. Swine Dysentery is a disease of the large intestine (colon) and this suggests that digestibility of the diet can affect the growth of the organism in the gut and the damage it subsequently does - the better the diet is digested in the small intestine, the less substrate will pass down the gut on which the organism will thrive. Diets with high levels of non-starch polysaccharides tend to induce more scour (with or without SD) as do pelleted diets compared to meal feeding.
Individual pigs that survive infection can range from fully recovered to chronically stunted with permanent diarrhoea. In recent years, 'milder' strains of Brachyspira hyodysenteriae have been recognised which present more as a low grade, cow-pat like, grower scour than as frank dysentery. (Fig 4). However, these strains appear to have the ability to 'drift' within a population, causing variable levels of disease.

Fig 3: Chronically stunted pig typical of SD without recovery

Fig 4: Cow pat like scour seen with grower scours (colitis) and mild SD
Diagnosis
Swine dysentery should be suspected in any situation where spreading scour is seen particularly in growing pigs, and certainly where there is any sign of blood or mucous in the scour.
Post mortem examination of affected pigs- either freshly dead by natural causes of the disease or by euthanasia - will show signs typical of swine dysentery within the spiral colon - oedema within the gut wall with congestion with swollen lymph nodes (fig 5).
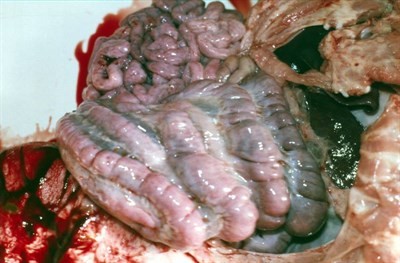
Fig 5: Oedema around the large intestine seen with SD
The inside lining of the large intestine (colon) will be inflamed, necrotic, blood streaked and with foul smelling material adhered to the surface. In milder cases the colon may only appear mildly congested and inflamed with watery grey contents. Of course, in the smaller populations where mortality does not occur, there is understandably a reluctance to sacrifice pigs for diagnostic purposes and if animals do not justify euthanasia on welfare grounds the diagnosis will be based on clinical signs supported by examination of faecal samples
The organism can be demonstrated in faeces, gut contents and mucosal scrapings by PCR tests - which have largely superseded a range of other laboratory tests. It is possible to see spiral organisms under the microscope in wet smears prepared from typically affected gut lining. However, this is not definitive for Brachyspira hyodysenteriae.
Other diseases that can mimic swine dysentery in the growing pig include Salmonella, Swine Fever, severe Spirochaetal diarrhoea (Brachyspira pilosicoli infection) and Trichuris suis infection (particularly a risk in outside conditions of prolonged occupation and contamination) whereas the less specific growers scours can arise as a result of dietary indigestion, chilling and infection with a wide range of organisms that include B. pilosicoli, Yersinia, E.coli, Salmonella and Lawsonia. Secondary invasion of the colon by Balantidium coli - a commensal gut parasite - can produce signs of blood and mucous making diagnosis complex.
A full veterinary investigation of suspect disease is always necessary.
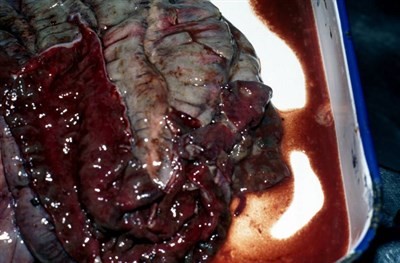
Fig 6: Severe haemorrhage and inflammation of the colon of a pig with SD
Treatment
Over the last few decades the range of treatments available for swine dysentery in the UK has declined both due to withdrawal of products (Carbadox, Arsenicals, Dimetridazole and Ronidazole) or by the development of variable levels of resistance to antibiotics (e.g. Tylosin).
Tiamulin and Lincomycin can be effective treatments given by injection or in water, and both of these products along with Valnemulin and Tylvalocin are available as in-feed products, which can be used at different levels, under veterinary direction, to effect treatment. As with any systemic disease, treatment of the sick pig by injection is essential and in the smaller populations may be the technique of choice for all pigs. However, there is an increasing concern that resistance to all of these antibiotics is increasing, potentially making treatment and control extremely challenging. Lincomycin had previously declined in efficacy following extensive use and the development of resistant strains but there has been some evidence that Brachyspira susceptibility has returned and may be effective where resistance to the pluromutilins (tiamulin & valnemulin) has occurred.
In the acute disease breakdown treatment must be selected on the basis of the veterinarian's clinical experience but for the longer term approach and certainly if medication eradication programmes are planned a full sensitivity picture is required. Disk diffusion tests to multiple antibiotics as used for many bacteria are not appropriate for B hyodysenteriae and difficult, lengthy and costly culture and minimum inhibitory concentration (mic) tests must be undertaken for each antibiotic separately.
Control
The primary aim for all herds is to prevent introduction into the unit which can be achieved by:
a) Attention to sourcing of stock
b) Care of moving pigs on and off the premises and quarantine on return
c) Attention to biosecurity particularly with relevance to anything that can carry faeces, including lorries (knackermen, stock hauliers and feed wagons)
d) Control of vermin and birds that can spread disease from farm to farm
e) Control of visitors
Siting of the herd well away from any other pigs is vital to avoid the risk of this and many other diseases. Equally proximity of an infected premises close to clean herds presents a big risk to them and the overall control of swine dysentery should at least consider a collaborative approach within an area as is currently encouraged by the AHDB Pork promoted Swine Dysentery charter.
Once present within the herd, the effects of disease must be carefully evaluated. In most cases, the depressant effect on performance and high costs of continual high level medication make the herd unsustainable. However, where it is feasible to live with swine dysentery ie in very mild disease situations, hygiene standards must remain high at all times. Strict 'all in, all out' procedures interspersed with thorough cleaning and disinfection, with or without lime washing, is vital. However, due to increasing antibiotic resistance and the general climate of responsible use of antibiotics and reducing pig farm dependency on antibiotic medication, SD is a disease with which it is very difficult to live in the long term.
The movement sale of weaners from a known infected site should be discouraged as it will spread disease to other localities maintaining and increasing risk to other farms. However carefully selected isolated premises can be used to facilitate a partial depopulation as part of an elimination programme.
Where ground becomes contaminated it may be necessary to abandon it for up to 6 months to allow natural decay of the organism.
Effective vaccines are not currently available.
Complete slaughter of the herd followed by a specific cleaning and disinfection programme before restocking with pigs from a SD free source is the most reliable way of eliminating the disease. However, short term high dose medication in combination with cleaning and disinfection and partial depopulation can be successful in eliminating the disease from an existing population. Medication should be chosen based on m.i.c assessment of the isolate from the farm. Such programmes can be tailored to the overall health picture of the farm and may allow elimination of other diseases at the same time using appropriate combination treatments and vaccines. Sarcoptic mange, Mycoplasma hyopneumonia, Actinobacillus pleuropneumoniae and PRRS can all be drawn into such elimination strategies.
Conclusion
Swine dysentery remains a major threat to UK pigs. It's diagnosis is complex, requiring full veterinary involvement, but its variability and appearance of less severe forms of the disease has led to some producers regarding it as a 'live with' disease. Within smaller stable populations can be achieved but the risks to the locality should always be considered along with antibiotic resistance and responsible use considerations.

